Sleep apnea test in Bakersfield, Ca
Pulmonary diagnoses
From COVID-19 to Pulmonary Hypertension, we specialize in an expansive range of pulmonary diagnoses, offering comfort and expertise every step of the way.
Our Pulmonary DIAGNOSES
Asthma
Asthma is a chronic respiratory condition that affects millions of people worldwide and is characterized by inflammation and narrowing of the airways, leading to recurrent episodes of wheezing, coughing, and shortness of breath. It is a complex and variable disease, with symptoms that can range from mild and occasional to severe and persistent. Asthma can be triggered by a variety of factors, including allergens like pollen or dust mites, respiratory infections, physical activity, or exposure to irritants such as smoke or air pollution. For many individuals, especially children, asthma symptoms can significantly impact their daily lives, limiting their ability to engage in physical activities or even perform routine tasks.
Effective asthma management typically involves a combination of long-term control medications to reduce airway inflammation and bronchodilators to relieve acute symptoms during asthma attacks. Education plays a crucial role in asthma care, as individuals with asthma and their families need to learn how to recognize triggers, administer medications correctly, and create an asthma action plan to respond to worsening symptoms. With proper management and adherence to treatment, most people with asthma can lead active, fulfilling lives and minimize the impact of this chronic condition on their overall well-being. Regular check-ups with healthcare providers are essential to assess asthma control and adjust treatment plans as needed to achieve optimal lung function and symptom control.
COPD
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease characterized by chronic airflow limitation and difficulty breathing. This progressive disease encompasses two main conditions: chronic bronchitis and emphysema, often coexisting in affected individuals. COPD is primarily caused by prolonged exposure to harmful irritants, such as cigarette smoke, air pollution, occupational dust, and chemicals. Over time, these irritants lead to inflammation and damage to the airways and air sacs within the lungs, resulting in reduced airflow and impaired lung function.
Symptoms of COPD typically include a persistent cough, often accompanied by increased mucus production, wheezing, shortness of breath (particularly during physical activity), and chest tightness. These symptoms can significantly impact a person’s quality of life, limiting their ability to engage in routine activities and even affecting their emotional well-being. Although COPD is a chronic and progressive condition, early diagnosis and appropriate management can help slow its progression, alleviate symptoms, and enhance the patient’s overall quality of life. Treatment options often include lifestyle modifications such as smoking cessation, pulmonary rehabilitation, bronchodilator medications, inhaled corticosteroids, and oxygen therapy in advanced cases. Efficiently managing COPD and enhancing the long-term outlook for individuals with obstructed airflow and breathing difficulties requires regular medical monitoring and adherence to treatment plans. This condition includes conditions like chronic bronchitis and emphysema. COPD is often caused by long-term exposure to irritants like cigarette smoke, air pollution, or occupational dust. Symptoms include a chronic cough, shortness of breath, and wheezing.
While there is no cure for COPD, various treatments, including medications and pulmonary rehabilitation, can help manage symptoms and improve patients’ quality of life. Quitting smoking and avoiding lung irritants are critical steps in preventing COPD or slowing its progression.
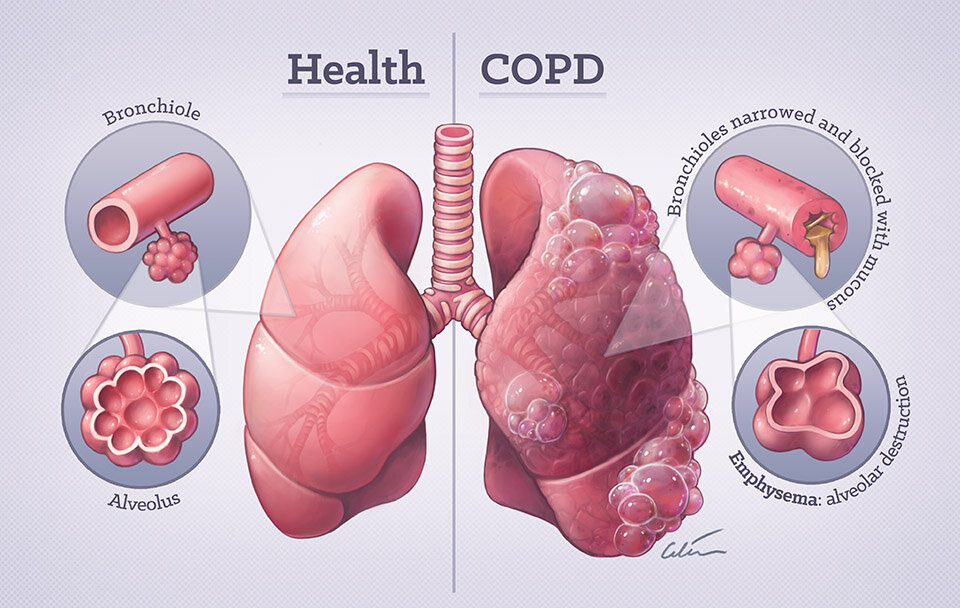
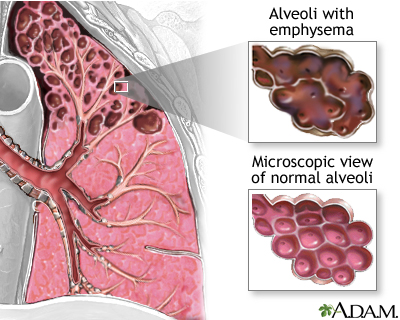
Emphysema
Emphysema is a chronic lung disease that falls under Chronic Obstructive Pulmonary Disease (COPD). It is characterized by the progressive deterioration of the air sacs (alveoli) in the lungs, leading to their damage and enlargement. The primary cause of emphysema is long-term exposure to lung irritants, with cigarette smoke being the most common and potent irritant. Occupational exposure to dust, chemicals, and air pollution can also contribute to the development of emphysema. As these irritants are inhaled over time, they trigger inflammation in the airways and release enzymes that break down the elastic fibers that provide support to the alveoli. This leads to a loss of elasticity in the lungs and results in a situation where the air sacs can’t effectively push air out during exhalation, trapping stale air in the lungs and making it difficult for individuals with emphysema to breathe.
Symptoms of emphysema often develop slowly and may include chronic coughing, wheezing, shortness of breath (particularly during physical activity), and chest tightness. As the condition progresses, these symptoms tend to worsen, and individuals may find it increasingly challenging to engage in routine daily activities. Emphysema is a progressive disease, and while it cannot be completely cured, there are treatments available to manage its symptoms and slow its progression. Lifestyle changes like quitting smoking, avoiding lung irritants, and adopting a healthier diet can be immensely beneficial. Medications, such as bronchodilators and inhaled corticosteroids, are often prescribed to open airways and reduce inflammation. In severe cases, surgical options like lung volume reduction surgery or lung transplantation may be considered to improve lung function and quality of life. Early diagnosis and a proactive approach to managing emphysema are essential to maintaining the best possible respiratory health for those affected by this condition.

COVID-19
COVID-19 is a highly contagious respiratory illness caused by the novel coronavirus SARS-CoV-2.It is primarily transmitted through respiratory droplets when an infected person coughs, sneezes, or talks, making close contact with infected individuals a significant risk factor.
The symptoms of COVID-19 can range from mild to severe and may include fever, cough, shortness of breath, fatigue, loss of taste or smell, and body aches. Severe cases can lead to pneumonia and acute respiratory distress syndrome (ARDS), which may require hospitalization and mechanical ventilation. Preventive measures, such as mask-wearing, physical distancing, hand hygiene, and vaccination, have played a crucial role in slowing the spread of the virus. The development and distribution of COVID-19 vaccines have been monumental efforts in curbing the pandemic, offering hope for eventual control and the return to a more normal way of life. However, the virus continues to evolve, and public health measures and ongoing research remain essential in managing this global health crisis.
Long-term COVID syndrome
Long-term COVID syndrome, often referred to as “Long COVID” or “post-acute sequelae of SARS-CoV-2 infection” (PASC), has emerged as a perplexing and concerning phenomenon in the wake of the COVID pandemic. While many individuals recover from the acute phase of the disease within a few weeks, a significant number continue to experience a range of debilitating symptoms for weeks, months, or even longer after their initial infection. These symptoms can vary widely and affect various organ systems, making Long COVID a complex and challenging condition to understand and manage.
Common symptoms of Long COVID include extreme fatigue, brain fog, shortness of breath, chest pain, joint pain, and heart palpitations, among others. Individuals with Long COVID often report a rollercoaster of symptoms that may come and go or evolve over time. This unpredictability can be deeply distressing as patients grapple with a diminished quality of life and the uncertainty of when, or if, they will fully recover. Medical professionals and researchers are actively studying Long COVID to unravel its underlying mechanisms, identify effective treatments, and provide better support to those affected. Long COVID serves as a stark reminder of the complexity and long-lasting impact of COVID, emphasizing the need for ongoing research and comprehensive healthcare approaches to address the diverse needs of patients experiencing this condition.

Valley Fever
Valley Fever is a fungal infection caused by inhaling airborne spores of the fungus Coccidioides immitis or Coccidioides posadasii. This disease is prevalent in arid and semi-arid regions of the southwestern United States, Mexico, and parts of Central and South America. The name “Valley Fever” is derived from its high incidence in the San Joaquin Valley of California, one of the most affected areas. When the spores become airborne due to soil disruption, such as through construction or windstorms, people in the vicinity can inhale them into their lungs, potentially leading to infection.
Valley Fever can manifest in various ways, with symptoms ranging from mild to severe. Many individuals exposed to the fungus may remain asymptomatic, while others experience flu-like symptoms such as fever, cough, fatigue, and chest pain. In some cases, especially among individuals with weakened immune systems, Valley Fever can progress to severe pneumonia and may even spread to other parts of the body, leading to complications. Although the majority of infections resolve on their own without specific treatment, antifungal medications may be necessary for severe cases or those with risk factors. Awareness of Valley Fever is crucial, particularly in regions where it is endemic, to ensure timely diagnosis and appropriate management of this fungal infection.

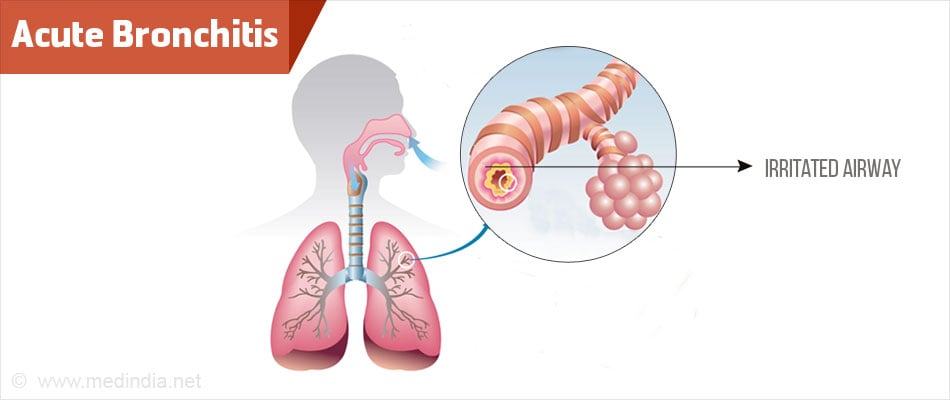
Bronchitis
Bronchitis is a common respiratory condition characterized by the inflammation of the bronchial tubes, which are responsible for carrying air to and from the lungs. This inflammation can result from viral or bacterial infections, exposure to irritants like tobacco smoke or pollutants, or underlying health conditions. There are two main types of bronchitis: acute and chronic. Acute bronchitis typically develops as a result of a viral infection, such as the common cold or influenza. It is characterized by symptoms like a persistent cough, the production of mucus, chest discomfort, and sometimes a low-grade fever. While acute bronchitis can be uncomfortable and disruptive, it often resolves on its own within a few weeks with rest and adequate hydration. However, it’s crucial to distinguish it from chronic bronchitis, a long-term condition associated with conditions like chronic obstructive pulmonary disease (COPD). Chronic bronchitis is defined by a persistent cough and mucus production for at least three months a year for two consecutive years, and it often requires ongoing management to alleviate symptoms and prevent complications.
Bronchitis is primarily diagnosed through a physical examination, a medical history review, and sometimes chest X-rays or other imaging tests. Treatment for acute bronchitis typically focuses on relieving symptoms and may involve rest, hydration, over-the-counter cough suppressants, and pain relievers. Antibiotics are usually not prescribed for viral cases but may be considered for bacterial infections. Chronic bronchitis, often associated with smoking, requires a more comprehensive approach. It involves smoking cessation as the most crucial step in halting the progression of the condition. Additionally, bronchodilators, corticosteroids, and pulmonary rehabilitation programs may be recommended to manage chronic bronchitis symptoms and improve lung function. Proper management and lifestyle changes can significantly enhance the quality of life for individuals living with bronchitis, reducing the frequency and severity of flare-ups.
Lung Cancer
Lung cancer is a malignant tumor that begins in the lungs, most commonly in the cells lining the airways. It ranks as one of the leading causes of cancer-related deaths worldwide, affecting both men and women. Lung cancer is often associated with tobacco smoking, as cigarette smoke contains numerous carcinogens that can damage lung tissue over time. However, non-smokers can also develop lung cancer, and it can result from exposure to other environmental factors, such as secondhand smoke, radon gas, asbestos, and air pollution.
The symptoms of lung cancer can vary but often include a persistent cough, chest pain, unexplained weight loss, shortness of breath, and coughing up blood. Detecting lung cancer at an early stage is crucial for improving treatment outcomes, but it is often diagnosed at advanced stages when the disease has already spread to other parts of the body. Treatment options for lung cancer depend on the type and stage of the disease and may include surgery to remove tumors, radiation therapy, chemotherapy, targeted therapies, and immunotherapy. Lung cancer remains a significant public health concern, emphasizing the importance of smoking cessation, regular screenings for individuals at high risk, and ongoing research to develop more effective treatments.

Pneumonia
Pneumonia is an inflammatory lung condition typically caused by infections, including bacteria, viruses, and fungi. It results in the air sacs in the lungs filling with pus or other fluids, leading to symptoms such as fever, cough, chest pain, and difficulty breathing. The severity of pneumonia can range from mild cases that resolve with rest and antibiotics to severe cases that require hospitalization, especially among vulnerable populations such as the elderly, young children, and individuals with weakened immune systems. In some instances, pneumonia can lead to complications like pleural effusion (accumulation of fluid around the lung), lung abscess, or respiratory failure, emphasizing the importance of early diagnosis and appropriate treatment.
The diagnosis of pneumonia often involves a physical examination, a chest X-ray, and sometimes additional tests such as blood cultures or sputum analysis to determine the underlying cause. Treatment depends on the specific pathogen responsible for the infection, with antibiotics prescribed for bacterial pneumonia, antiviral medications for viral pneumonia, and antifungal drugs for fungal pneumonia. Adequate hydration, rest, and supportive care are also essential components of recovery. Prevention strategies include vaccination against common bacterial and viral causes of pneumonia, practicing good hand hygiene, and avoiding exposure to known lung irritants like cigarette smoke. Prompt medical attention and adherence to prescribed treatments are critical for managing pneumonia effectively and preventing complications.
Snoring
Snoring is a common sleep-related sound caused by the vibration of tissues in the throat and upper airway. It occurs when the flow of air through the mouth and nose is partially obstructed, leading to the generation of sound as the air passes through the narrowed passage. While snoring is generally considered a harmless and widespread occurrence, it can often disrupt the sleep of both the person who snores and their sleeping partner. The intensity and frequency of snoring can vary widely from person to person, with some individuals producing only mild, occasional sounds, while others may snore loudly and consistently throughout the night.
Snoring can result from a variety of factors, including the relaxation of throat muscles and tissues during sleep, excess weight, nasal congestion, or the consumption of alcohol or sedatives before bedtime. In some cases, snoring may be indicative of an underlying sleep disorder, such as obstructive sleep apnea (OSA), a condition where breathing repeatedly stops and starts during sleep. While snoring itself is usually not a cause for medical concern, chronic and disruptive snoring should not be ignored, as it can affect the quality of sleep, lead to daytime fatigue, and strain relationships. If snoring is a persistent issue or is accompanied by other symptoms like choking or gasping during sleep, it’s advisable to consult a healthcare professional to rule out underlying sleep disorders and explore potential solutions for more restful and quiet nights.
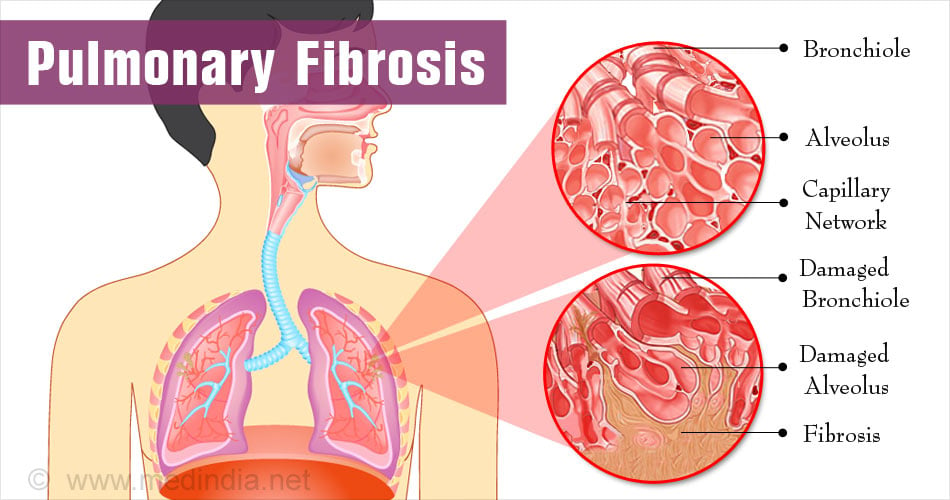
Pulmonary Fibrosis
Pulmonary Fibrosis is a progressive lung disease characterized by the gradual scarring and thickening of lung tissues. This scarring, known as fibrosis, makes it increasingly difficult for the lungs to function effectively, leading to impaired oxygen exchange and ultimately causing breathlessness and reduced lung capacity. Pulmonary Fibrosis can result from various factors, including exposure to environmental toxins, occupational hazards, certain medications, and autoimmune disorders. However, in many cases, the exact cause remains unknown, and such cases are referred to as idiopathic pulmonary fibrosis (IPF).
Individuals with Pulmonary Fibrosis often experience a persistent dry cough, shortness of breath, and fatigue, which can significantly impact their daily lives and overall well-being. As the disease progresses, these symptoms tend to worsen, making it challenging to perform even routine activities. While there is currently no cure for Pulmonary Fibrosis, medical interventions and treatments are available to slow the disease’s progression, alleviate symptoms, and improve the quality of life for affected individuals. These treatments may include medications to reduce inflammation and fibrosis, supplemental oxygen therapy to enhance oxygen levels, and pulmonary rehabilitation programs to enhance physical endurance. In some severe cases, lung transplantation may be considered a viable option to extend life expectancy and improve respiratory function. Close monitoring by healthcare professionals and a supportive care team is essential for managing Pulmonary Fibrosis and optimizing the quality of life for those affected by this challenging condition.
Interstitial Lung Disease
Interstitial Lung Disease (ILD) encompasses a diverse group of over 200 lung disorders characterized by inflammation and scarring of the lung tissue, specifically the interstitium, which is the space between the air sacs in the lungs. This condition disrupts the normal functioning of the lungs, making it increasingly challenging for affected individuals to breathe. While the causes of ILD can vary, it often results from exposure to environmental toxins, such as asbestos or silica dust, autoimmune diseases like rheumatoid arthritis or systemic sclerosis, and infections. In some cases, the exact cause remains unknown, leading to the term “idiopathic interstitial lung disease.”
Symptoms of ILD typically include persistent dry coughs, shortness of breath, and reduced exercise tolerance. As the condition progresses, individuals may experience fatigue and chest discomfort. Diagnosis involves a combination of medical history, physical examination, imaging studies like high-resolution computed tomography (HRCT) scans, and sometimes lung biopsies to determine the specific type and severity of ILD. Once diagnosed, treatment options vary depending on the underlying cause and the stage of the disease. Medications, including corticosteroids and immunosuppressants, are often used to reduce inflammation and slow the progression of scarring. Pulmonary rehabilitation, supplemental oxygen therapy, and lung transplants may also be considered in advanced cases. Given the complexity of ILD, a multidisciplinary approach involving pulmonologists and rheumatologists is essential to provide comprehensive care and improve the quality of life for individuals affected by this challenging condition.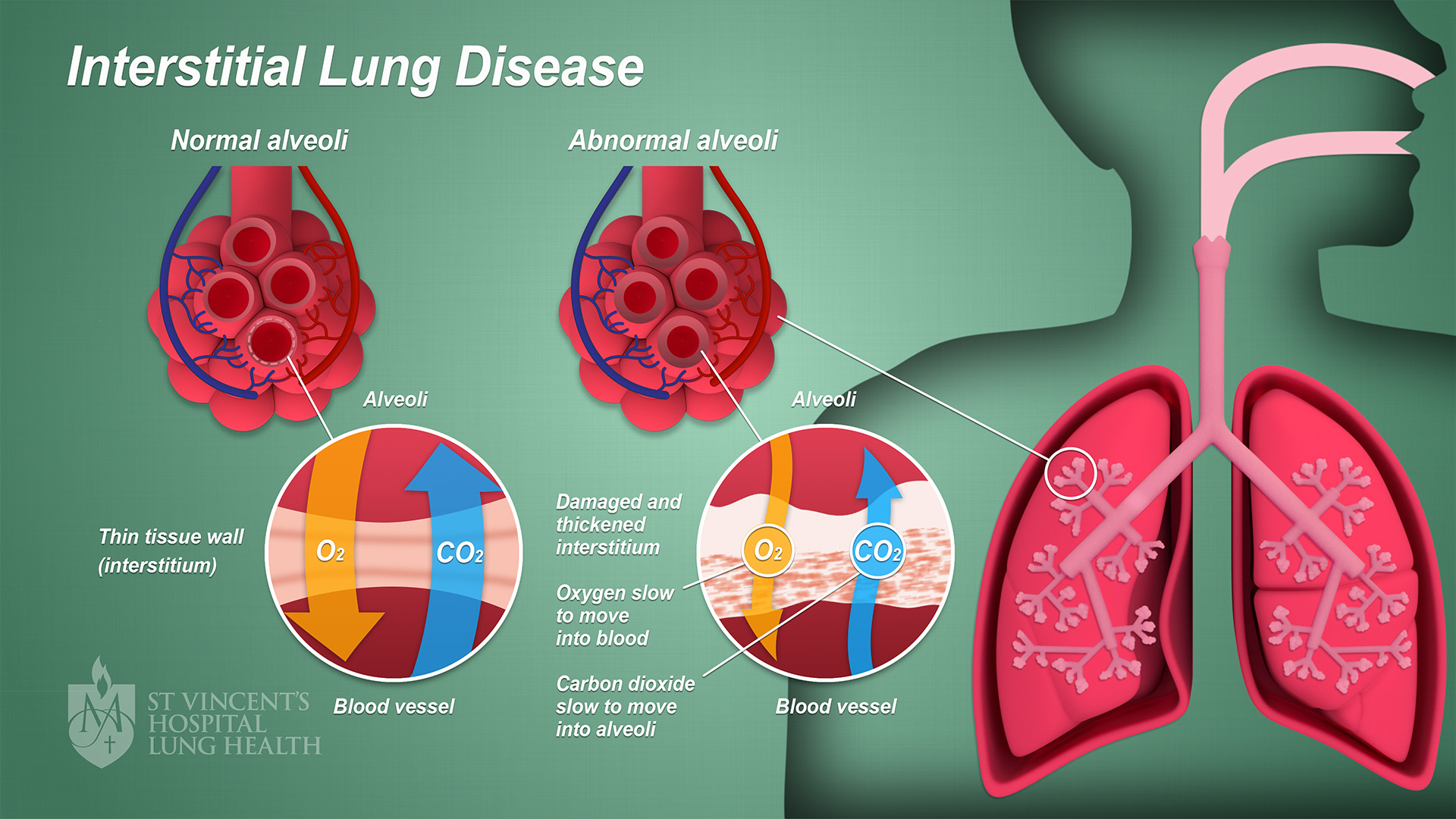
ALS (Amyotrophic Lateral Sclerosis)
Amyotrophic Lateral Sclerosis (ALS), often referred to as Lou Gehrig’s disease, is a relentlessly progressive and devastating neurodegenerative disorder that primarily affects the motor neurons in the brain and spinal cord. This debilitating condition leads to the gradual degeneration and loss of these motor neurons, which are responsible for controlling voluntary muscle movements. As a result, individuals with ALS experience a relentless decline in muscle strength, coordination, and function. Early symptoms may include muscle weakness, twitching, and cramps, often in one limb, but they eventually spread to other parts of the body. As the disease advances, individuals may face difficulty speaking, swallowing, and breathing, ultimately leading to respiratory failure, which is the most common cause of death among ALS patients.
ALS is a particularly challenging condition to manage. However, supportive care and treatments can help alleviate symptoms, prolong survival, and improve the quality of life for those living with ALS. A multidisciplinary approach involving neurologists, physical and occupational therapists, speech-language pathologists, and respiratory therapists is typically employed to address the diverse needs of ALS patients. Additionally, assistive devices, such as wheelchairs and communication aids, can help individuals maintain their independence and communication abilities for as long as possible. Ongoing research into the causes and potential treatments for ALS is vital, and organizations worldwide are dedicated to finding a cure and better therapies for this debilitating disease.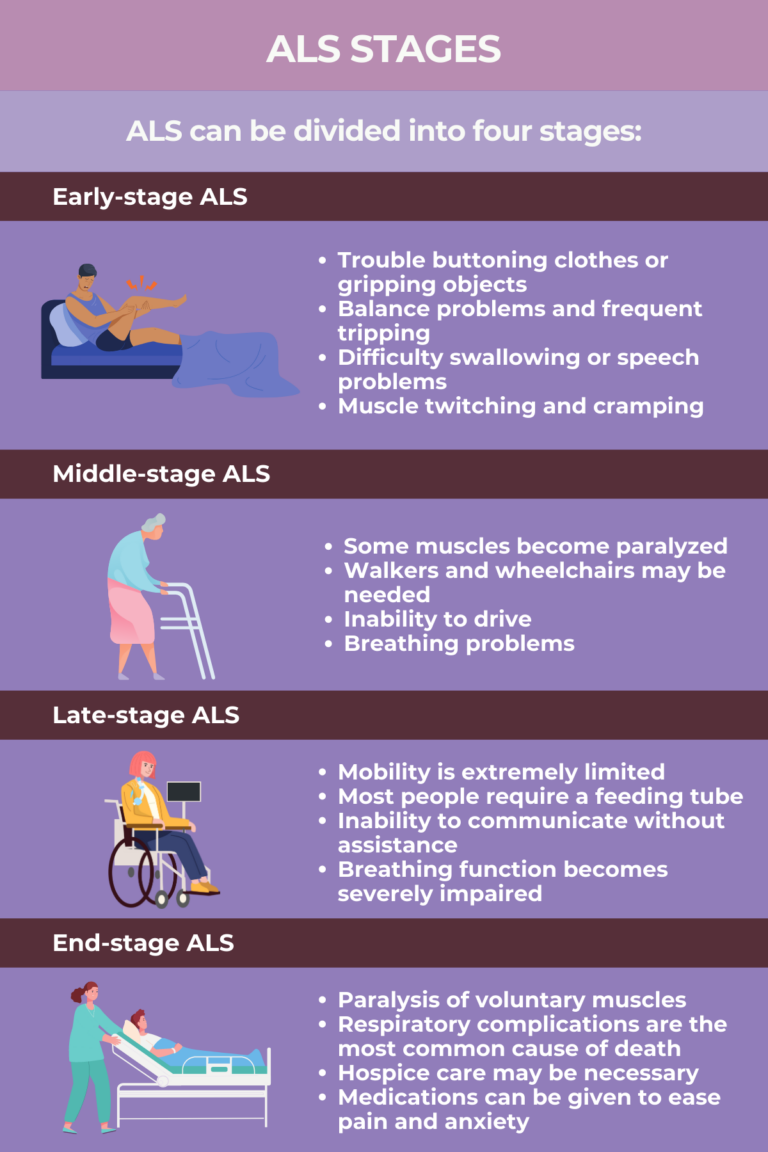
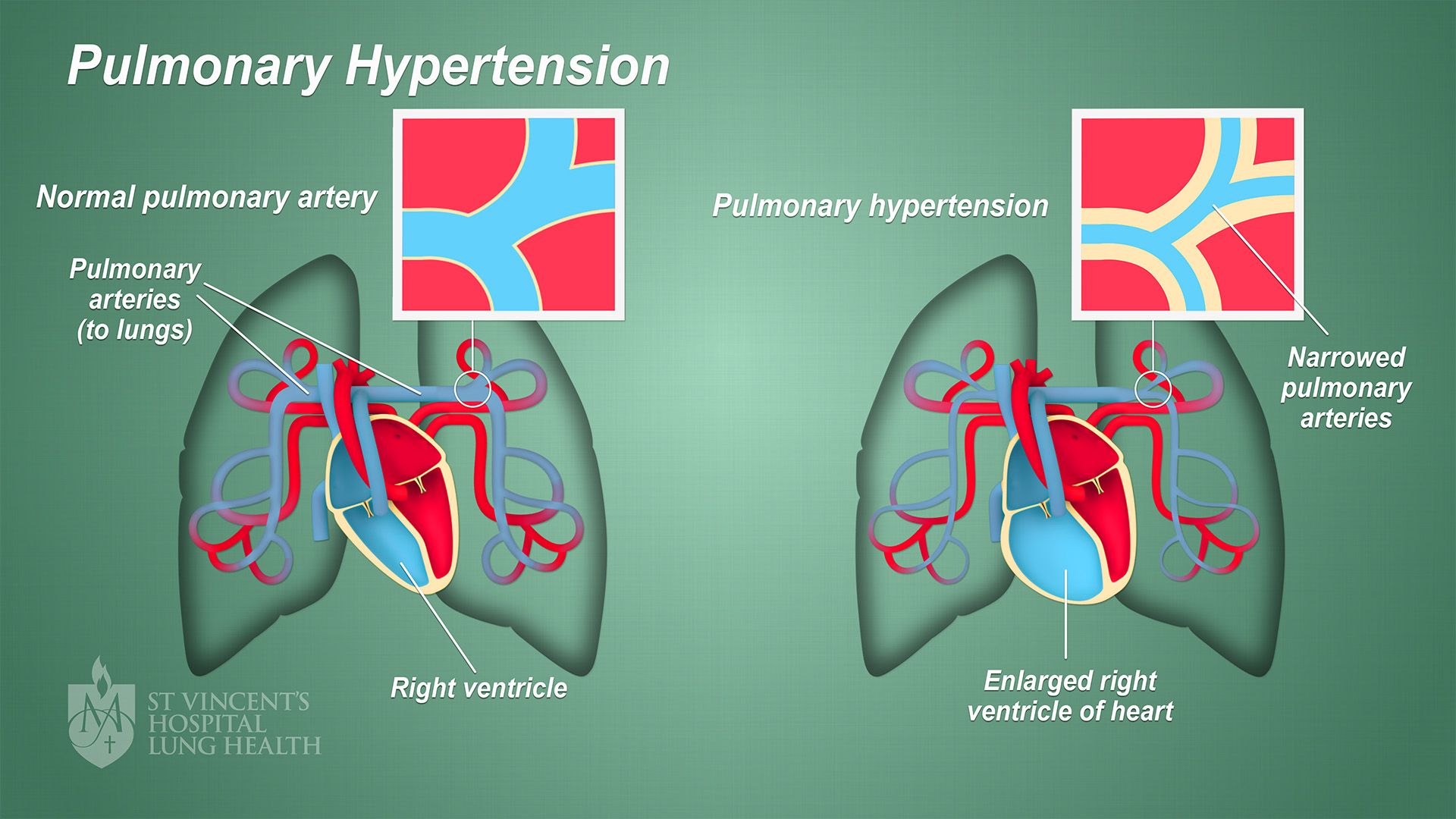
Pulmonary Hypertension
Pulmonary Hypertension (PH) is a complex and relatively rare medical condition characterized by elevated blood pressure in the arteries that supply the lungs. Pulmonary hypertension specifically targets the pulmonary arteries, leading to increased resistance in these vessels. As a result, the right side of the heart must work harder to pump blood through the lungs, which can ultimately lead to heart failure if left untreated. PH can be classified into several groups based on its underlying causes, including idiopathic (unknown cause), hereditary, and secondary forms related to conditions such as connective tissue diseases, congenital heart defects, or chronic lung diseases.
The symptoms of pulmonary hypertension can be insidious and often nonspecific, making early diagnosis challenging. Common symptoms include shortness of breath, fatigue, chest pain, and fainting episodes. Over time, individuals with PH may experience a reduced ability to participate in physical activities due to worsening breathlessness. Diagnosis typically involves a combination of medical history, physical examination, imaging tests like echocardiography, and right heart catheterization to measure the pressure in the pulmonary arteries directly. While there is currently no cure for PH, advances in treatment options have significantly improved the prognosis for many patients. Medications designed to dilate blood vessels and reduce blood pressure in the pulmonary arteries, such as vasodilators and endothelin receptor antagonists, are often prescribed to manage the condition. Additionally, oxygen therapy and lifestyle modifications can help improve patients’ quality of life and slow the progression of the disease. Close monitoring by a specialized healthcare team is essential to tailor treatment plans and provide ongoing support to individuals living with pulmonary hypertension.
Pulmonary Infections
Pulmonary infections refer to infections that affect the respiratory system, including the lungs. Common causes include bacteria, viruses, and fungi. These infections can range from mild illnesses like bronchitis to severe conditions like pneumonia. Symptoms often include coughing, fever, chest pain, and difficulty breathing.
Pulmonary infections depend on the specific pathogen causing the infection. Bacterial infections are typically treated with antibiotics, while antiviral medications are used for viral infections. Fungal infections may require antifungal drugs. Supportive care, including rest, hydration, and fever-reducing medications, can help alleviate symptoms and promote recovery. In severe cases, hospitalization may be necessary, especially when there is a risk of complications or if the infection is causing respiratory distress. Preventive measures, such as vaccination (for some viral and bacterial infections) and good hygiene practices, play a crucial role in reducing the risk of pulmonary infections. Early diagnosis and prompt treatment are essential for achieving the best outcomes and preventing the spread of these infections to others.
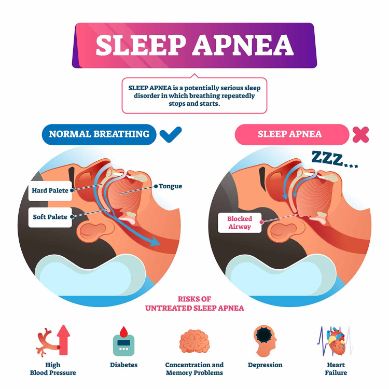
Sleep Apnea
Sleep apnea is a common sleep disorder characterized by recurrent interruptions in breathing during sleep. These interruptions, known as apneas, occur when the muscles in the throat relax excessively and temporarily block the airway. This results in a lack of oxygen reaching the lungs and subsequently the brain, leading to brief awakenings or arousal from sleep to restore normal breathing. While individuals with sleep apnea may not always be aware of these awakenings, they can happen many times throughout the night, severely disrupting the sleep cycle. This constant cycle of sleep disruption can lead to excessive daytime fatigue, impaired concentration, mood changes, and even cardiovascular problems over time.
There are two main types of sleep apnea: obstructive sleep apnea (OSA) and central sleep apnea (CSA). OSA, the more common form, occurs when the airway is physically blocked or narrowed due to factors such as excess weight, enlarged tonsils, or nasal congestion. CSA, on the other hand, results from a failure of the brain to send the appropriate signals to the muscles responsible for breathing. Effective treatment options for sleep apnea are available and may include lifestyle modifications such as weight loss, positional therapy, and avoiding alcohol and sedatives before bedtime. Additionally, continuous positive airway pressure (CPAP) machines and oral appliances can help keep the airway open during sleep. Proper diagnosis and treatment of sleep apnea is crucial to improving sleep quality, reducing daytime symptoms, and preventing long-term health complications.
Pulmonary embolism
Pulmonary embolism is a medical condition characterized by an abnormal accumulation of fluid in the pleural cavity, a space between the two layers of the thin membrane (pleura) that surrounds the lungs. This condition can result from a variety of underlying causes, including infections, congestive heart failure, malignancies, pulmonary embolisms, or trauma. As the fluid accumulates, it compresses the lung, preventing it from fully expanding during inhalation. This compression can lead to symptoms such as chest pain, shortness of breath, and a persistent cough.
The diagnosis of Pulmonary Embolism typically involves a combination of physical examinations, a medical history review, and imaging tests like chest X-rays or ultrasounds. Once diagnosed, treatment depends on the underlying cause and the amount of fluid present. Small effusions may resolve on their own when the underlying condition is treated, while larger or symptomatic effusions may require interventions such as thoracentesis (draining the fluid with a needle), pleurodesis (a procedure to fuse the pleura layers), or the placement of a chest tube to drain and manage the fluid. Managing pleural effusion effectively is essential to relieve symptoms and address the root cause, thereby improving a patient’s overall lung function and quality of life.
Contact Us
Visit Us
5531 Business Park S, Suite 201a
Bakersfield, CA 93309
Hours
Mon-Fri: 9 am-5 pm
Sat-Sun: Closed
